Almost 4 million babies are born in the United States every year. That’s nearly 11,000 newborns a day. In some respects, it’s the safest it’s ever been to give birth in this country, with improvements in technologies and medicines, and better prenatal monitoring of soon-to-be mothers.
But the U.S. today has the worst maternal mortality rate among any developed country—and that rate has been steadily rising, increasing by 26% between 2000 and 2014*. In some groups, the numbers are particularly startling: For every 100,000 live births, 40 African-American women die compared to 12.4 white women, according to the Centers for Disease Control and Prevention.
The reasons for the rise are complex says Penn sociologist Courtney Boen, who specializes in population studies. “It is partially attributed to better surveillance,” she says. Boen also cites an increase in medically complicated pregnancies as a potential factor, due in part to more older women having babies.
Deborah Driscoll, chair of Penn Medicine’s Obstetrics and Gynecology Department, notes that an increase in the prevalence of pre-diabetes, diabetes, obesity, and opioid use during pregnancy has also played a role.
A mother’s death is classified as a “maternal mortality” for up to a year after she gives birth, and half of such deaths happen after the mother has delivered and left the hospital postpartum. Beyond that, many of the causes are well known, including heart failure and hypertension, as well as complications from anesthesia, venous thromboembolism, or failure to receive timely blood transfusions in the event of hemorrhage.
Despite knowing what we do about this challenge, the uptick in losses continues at national and local levels, and disproportionately for some groups. At Penn, experts are studying and addressing maternal mortality head on. Initiatives at the Perelman School of Medicine, for instance, focus on aspects of postpartum care like monitoring a new mom’s blood pressure once she’s home, as well as educating clinical staff. And the Office of Inclusion and Diversity is working to address health inequity and racial bias baked into the system. It’s all part of a movement to recognize the role that social determinants, socioeconomics, and racism play.
“Maternal mortality in general, especially in the U.S., involves so many facets of a woman’s life,” says Monique Shaw, a fellow at Penn’s Center for Public Health Initiatives. “When we look at social determinants of health, access to prenatal and postnatal support, institutional racism, or even a zip code where someone lives, all of these contribute to maternal mortality and the disparity we’re seeing, particularly for African-American women.”
Giving birth at home
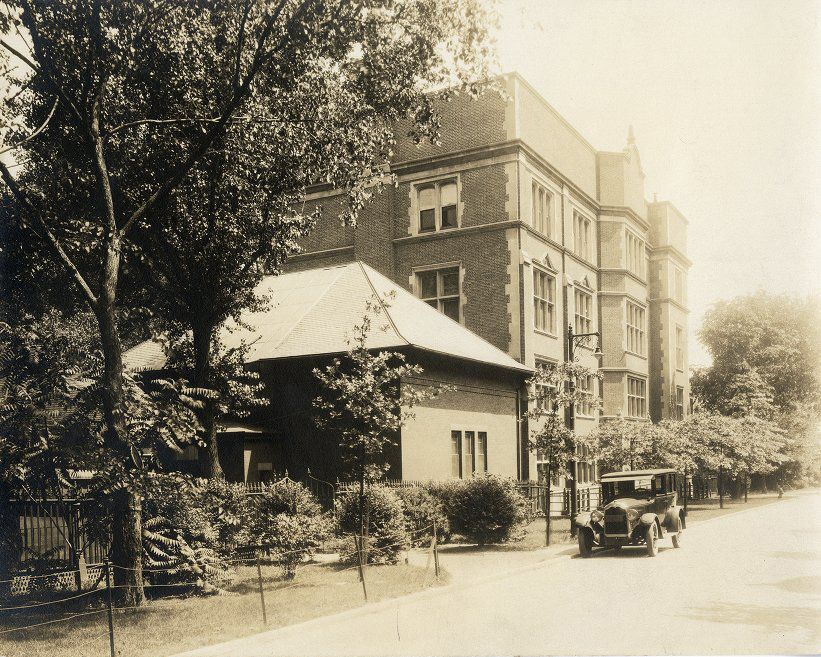
To understand how giving birth has changed in the United States requires looking back to a time when most women did so at home rather than at a hospital, before the turn of the 20th century. “Back then, women just didn’t want to come to the hospital. They were so afraid of infection,” Driscoll says. “They’d have high fevers and would be given a shot of whiskey and a cold compress to bring down their fever, but there was no Tylenol. There were no antibiotics.”
At that time, this idea of protection against germs was a relatively new phenomenon.
Women placed in close hospital quarters would often contract and sometimes die from afflictions like puerperal sepsis, an infection of the genital tract that’s still one of the top five causes of maternal mortality today. Antibiotics wouldn’t come into the picture for another two-plus decades, but in the late 19th and early 20th centuries, care providers knew something had to change.
“They became more and more aware that you needed what they would call an ‘aseptic environment,’ or what we would call ‘sterile,’” says Patricia D’Antonio, director of the Barbara Bates Center for the Study of the History of Nursing in Penn’s School of Nursing.
There was also a growing understanding that safe birth meant more than just safe delivery conditions, that the health of mother and baby required monitoring throughout the gestational period. Doctors and nurses began to see that high blood pressure and higher incidence of protein in the mother’s urine mattered and could be dangerous. “Gradually,” D’Antonio says, “the importance of prenatal care started to emerge.”
That meant a change in thinking about the birthing process, she adds. “Nurses and physicians had to transform the popular conception of childbirth from a natural event to a physiological process that could put lives in danger.” They enlisted trusted community members like nurses and religious leaders, plus the fathers themselves, educating them about the need for prenatal care.
Eventually the shift took hold, bolstered by the widespread use of antibiotics after World War II and technological advances in health care. Though the number is now trending upward, today fewer than 2% of births in the United States happen outside of a hospital setting.
The racial gap
Childbirth in a hospital doesn’t automatically mean equal care or similar maternal mortality rates for all groups. In fact, black women are three to four times more likely to die from childbirth than white women from complications related to cardiovascular disease, preeclampsia, and eclampsia. That number hasn’t budged in six decades.
Socioeconomic status doesn’t change the trajectory either, adds Sindhu Srinivas, HUP’s director of obstetrical services and vice chair for quality and safety for the Obstetrics and Gynecology Department. Case in point: One study conducted by the New York City Department of Health and Mental Hygiene found that black women with a college degree had higher rates of maternal mortality than white high-school dropouts.
“Black women are exposed to racism well before they get pregnant,” Boen says. “With the histories and discrimination they experience, black women enter pregnancy with higher rates of hypertension, then we see racial bias in the health care system.”
It’s this prejudice that a Penn Medicine team led by Eve Higginbotham, vice dean for inclusion and diversity and a professor of ophthalmology, is working to address by analyzing disparities in wait times in the emergency room, as well as in the way providers view the workplace, their patients, and their colleagues. Higginbotham’s team is also trying to understand the biases underlying maternal health care, like the notion that doctors and nurses ignore fears black women raise about their health or the social factors at work. (Even Serena Williams, despite her high profile as an athlete, experienced this, speaking out about how her postpartum team did not take seriously her concerns about potentially lethal blood clots.)
For the past three years, scores of faculty and staff have attended workshops put on by the Penn Medicine Office of Inclusion and Diversity focused on increasing self-awareness regarding unconscious bias, Higginbotham notes. “Bias in the delivery of care, both structurally and individually,” she says, “contributes to disparities in maternal morbidity rates as well as other disparities in health care.”
Such concerns are part of the reason Srinivas and Penn maternal fetal medicine physician Adi Hirshberg created a program at Penn called Heart Safe Motherhood. “For postpartum women with hypertension, doctors recommend blood pressure checks within 72 hours and again at 7 to 10 days after delivery. But office visits [often] have a poor show rate,” says Srinivas. Heart Safe Motherhood started sending each patient home with her own blood pressure cuff, asking her to text in blood pressure readings twice daily for 10 days post-discharge through a custom-developed messaging platform.
More than 90% of women shared their numbers, essentially eliminating the racial disparity in postpartum care at HUP. “We’ve been able to identify women through this program who may need to come back to the hospital or would require an early postpartum visit,” Driscoll says. “In general, we’re trying to focus on what we can do to mitigate the risk for maternal morbidity and mortality, to ensure we have the right protocols and guidelines in place for high-quality, safe care.”
To that end, Driscoll says that all staff go through postpartum hemorrhage training and the Health System also has a center of excellence for opioid use in pregnancy. Elsewhere at the University, researchers like Kimberly Trout of the Nursing School specialize in prenatal care, teaching the next generation of nurses and nurse midwives the skills that are key to improving a broken system for treating new mothers. “We’ve seen a decline in infant mortality and high-need, high-risk babies. But we don’t do a good job of taking care of high-risk moms,” Boen says. “Most women get discharged and aren’t required to see a doctor again for six weeks.”
‘Not an occurrence’
Despite the ongoing research at Penn and the strides made at the Health System to improve care for mothers, solving the challenge will require efforts beyond what any single hospital system or University can do. More tracking and better data are necessary, as is collaboration among clinicians, public-health advocates, hospital administrators, on-the-ground support like doulas or lactation consultants, and policymakers.
The Preventing Maternal Death Acts of 2018 became law in December of last year, with the aim of caring for mothers during pregnancy, childbirth, and the postpartum period. It had more than 190 co-sponsors from both parties.
Though the Act addresses the idea that women face social, economic, and racial disparities that don’t disappear at the doctor’s office or hospital bedside, Shaw says more effort is needed, starting with a different way of thinking about the process and those going through it.
“Our society views childbirth as something that happens and then it’s over, like an occurrence. That’s seen through organizational and federal policies,” she says. “That culture and mindset have to shift. Childbirth is not an occurrence that happens and is just over. It’s a life-altering experience and it takes women a very long time to recover and adjust.”
*The 26% applies to only 48 states; California and Texas, the two largest states, collectively account for about 20% of births in the U.S. With those states factored in, maternal mortality in U.S. as a whole rose by approximately 16% between 2000 and 2014.
Courtney Boen is an assistant professor in the Department of Sociology in the School of Arts and Sciences.
Patricia D’Antonio is the Carol E. Ware Professor in Mental Health Nursing, chair of the Department of Family and Community Health and director of the Barbara Bates Center for the Study of the History of Nursing in the School of Nursing. She is also a senior fellow at the Leonard Davis Institute of Health Economics.
Deborah Driscoll is the Luigi Mastroianni, Jr. Professor of Obstetrics and Gynecology and chair of the Obstetrics and Gynecology Department at the Perelman School of Medicine.
Eve Higginbotham is the vice dean for inclusion and diversity and a professor in the Department of Ophthalmology at the Perelman School of Medicine. She is also a senior fellow at the Leonard Davis Institute of Health Economics.
Mark Frazier Lloyd is director of the University Archives and Records Center.
Monique Shaw is a fellow at the Center for Public Health Initiatives and teaching faculty in the Master of Public Health program at the University of Pennsylvania. She is also a doctoral candidate at the University of the Sciences.
Sindhu Srinivas is director of obstetrical services and vice chair for quality and safety for the Obstetrics and Gynecology Department at the Perelman School of Medicine.