Anne Teitelman believes the key to helping women stay healthy is to meet them where they are, to bring the personal, health-related care into their daily lives, not sequester it to a once- or twice-a-year visit to a nurse practitioner, doctor, or another care provider. So, the Penn Nursing researcher built two apps.
The first, called Everhealthier Women, focuses on preventive health actions around cancers such as breast cancer and cervical cancer. The second, called NowIKnow, is aimed at getting 18- to 26-year-olds to complete the three-dose human papillomavirus (HPV) vaccine cycle. A special section in the November issue of The Journal of Obstetric, Gynecologic, & Neonatal Nursing that Teitelman guest-edited features papers on each, as well as a piece Teitelman wrote about using mobile technologies to improve women’s health.
“You’re trying to stay healthy every day. You’re trying to manage your health every day. That’s where health really happens,” says Teitelman, a nurse practitioner who researches global women’s health. “If you want to reach people with health messages in their day to day, a mobile application is a really good way to do that.”
Everhealthier Women came first, an answer to the challenge put out by the Office of Health Information Technology, an arm of the Department of Health and Human Services (HHS), for an app that would help women of color reduce their cancer risk. Though Teitelman had never developed an app, she already had a funded research project aimed at building an intervention for cervical cancer prevention among socioeconomically disadvantaged women.
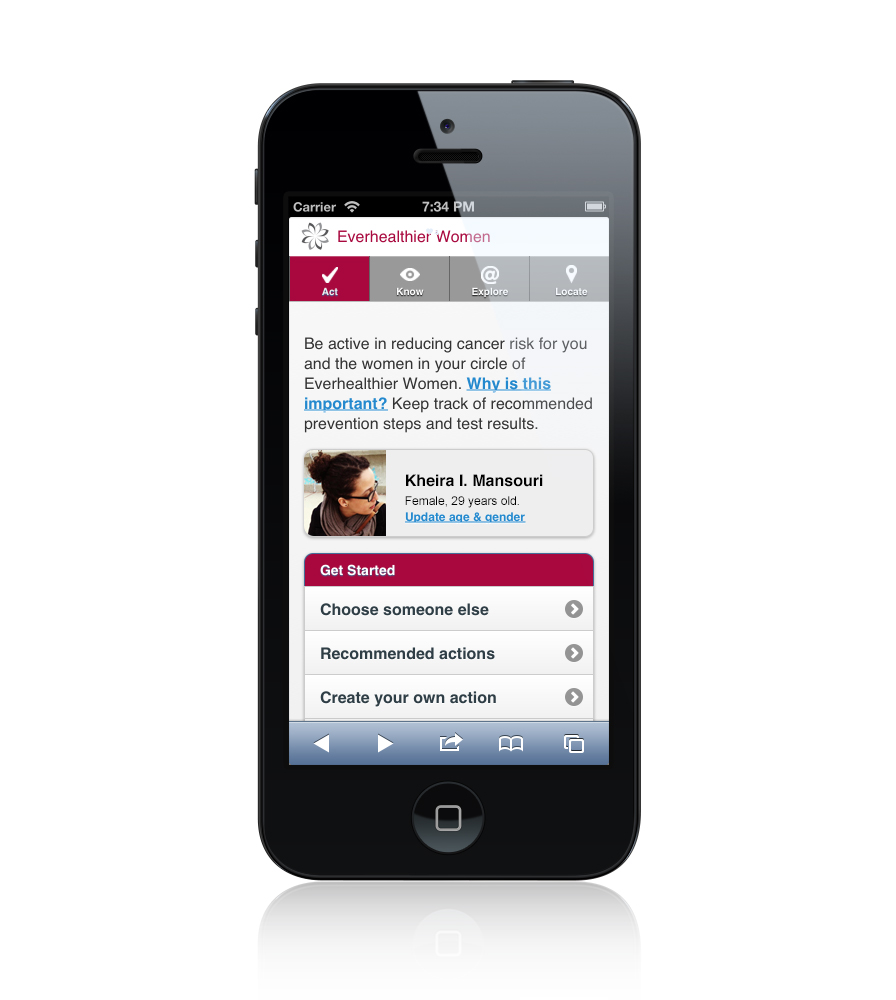
She worked with a developer to put together what would become Everhealthier Women. The web-based app has four main pages—Act, Know, Explore, and Locate—which allow users to track medical information like appointments and lab tests, send targeted messages to themselves and others in their circle, and read relevant content on social media. The locator tab pulls up nearby clinics by ZIP code.
“The whole premise is that women are busy and just trying to fit all of this into their lives, taking care of themselves and taking care of their loved ones,” Teitelman says.
Fifteen 18- to 30-year-old women tested Everhealthier Women once it went live. After completing a baseline survey about their use of technology in health care, they were introduced to the app, then, during the following three weeks, the research team elicited feedback. Despite a short study period, the researchers learned a good deal from participants. “The women felt a need for this, they thought they would use it, they liked the idea of it,” Teitelman explains. “They also felt this could really benefit them.”
In addition to earning the top prize from HHS in the app-development challenge, Teitelman’s app prodded her to take another stab at such a project, incorporating what she learned from the first go-round. For NowIKnow, she focused on HPV, the most common sexually transmitted infection in the United States and the leading cause of cervical cancer.
The Centers for Disease Control and Prevention recommends a two-dose HPV vaccine series for 11- to 14-year-olds (males and females) or a three-dose series within a six-month window for previously unvaccinated women 15 to 26 and men 15 to 21. Yet this often doesn’t happen; in 2015, just 42 percent of 19- to 26-year-old women had received the first one, with lower rates for black and Hispanic women compared to white women. Even if someone gets the initial shot, follow-up appointments may never materialize, perhaps because someone moved, has trouble finding the time, or can’t afford the return visit.
Teitelman wanted to zero in on what she saw as a missed opportunity, a gap in motivating women, especially women of color, to complete the vaccine series. After conducting theory-based elicitation research and after gathering preliminary input from a community advisory board, she and a group of undergraduate and graduate students from the School of Nursing and the Perelman School of Medicine identified a list of 12 salient beliefs to address via the app. For example, “Getting the HPV vaccine reduces the chances of developing cervical cancer,” and “My friends would approve of me getting the HPV vaccine.”
The team then built the mobile health intervention using the same approach Teitelman took with Everhealthier Women, bringing the health-care conversation to the daily lives of users, this time via a set of weekly stories written by the group with feedback from women in the community.
“We tried to make it really real, to include a lot of the day-to-day life of the women we were seeing,” Teitelman says. “The stories took place at the laundromat, on the stoop on a hot summer day, maybe in the clinic waiting room, sitting and watching TV at home, hearing that your aunt died of cervical cancer and being concerned about what that means for you.”
The research team tested the new app with 35 young women who lived in economically disadvantaged communities and had received the first dose of the vaccine. The researchers determined that using content tailored to a target population can potentially reduce cancer disparities by reaching these harder-to-reach populations.
That aligns well with Teitelman’s goals for this type of work in general.
“I’m interested in addressing health disparities, and cervical cancer really disproportionately affects minority women,” she explains. “If we don’t make extra efforts to connect with minority women, we’re going to worsen the health disparities by differentially distributing the prevention method. That’s what this app is about, to speak to the women who never got the vaccine as kids and who are now being offered it as adults and can make the decision. We’re trying to help them see the benefits.”
Teitelman has other projects in the works using similar tech-based mobile health interventions with input from the community, like one that sends text reminders to women to take a daily HIV prevention pill. It’s not the only type of research she conducts, but it’s one in which she sees great potential.
“If I want to be a nurse in the community, what am I going to do, go door to door?” she says. “I could develop an app and then I could reach people every day in the community, where they are, in their lives. That’s what I do.”
Anne Teitelman is the Patricia Bleznak Silverstein and Howard A. Silverstein Endowed Term Chair in Global Women’s Health, and an associate professor in the School of Nursing, as well as an associate professor of obstetrics and gynecology in the Perelman School of Medicine at the University of Pennsylvania.