On July 27, 1921, Canadian surgeon Frederick Banting and University of Toronto medical student Charles Best successfully isolated the hormone insulin for the first time. It marked one of the most important breakthroughs in the history of diabetic treatment. Within a year, people suffering from diabetes were being treated with insulin for a disease that had been considered fatal.
Penn Today talked to experts from across the University to hear their thoughts on the 100th anniversary of this medical breakthrough, from the discovery’s significance through the lens of history to the economics of insulin to the state of diabetes treatment today.
Chris Feudtner, pediatrician, clinical investigator, and ethicist at The Children’s Hospital of Philadelphia (CHOP) and professor of Pediatrics, Medical Ethics and Health Policy at the Perelman School of Medicine
Insulin is one of the leading medical miracles of the 20th century, on par with antimicrobials and cancer treatments. Prior to insulin’s discovery in 1921, children and adults who developed diabetes most often died within days to months, and perhaps a few years; with the advent of insulin therapy, this timeline was extended to decades.
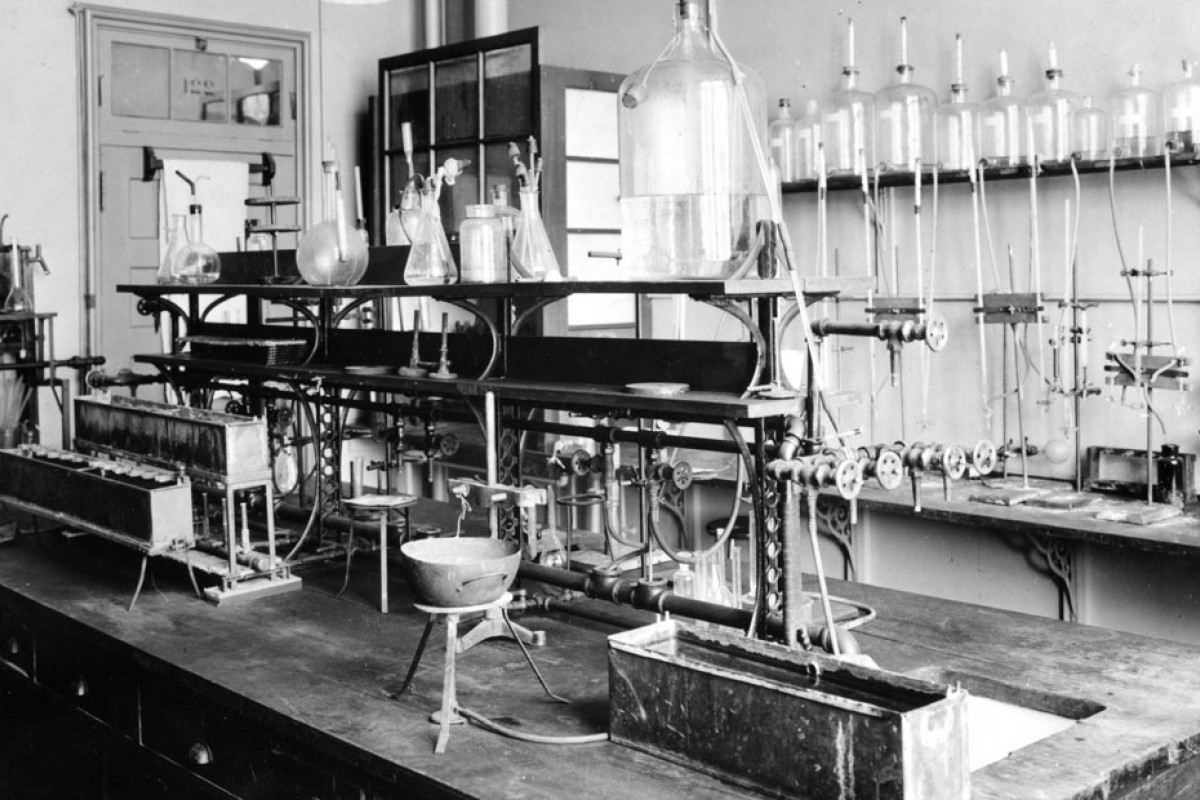
This August marks 100 years from the hot Toronto summer when Fred Banting and Charlie Best injected a pancreatic extract into a diabetic dog and documented the blood sugar fall. This is an event worth celebrating—yet we should also unpack three aspects of the history of insulin, each revealing an ironic contrast between what we believe and what happened, each posing an important question.
First, Banting and Best’s experimental approach was non-reproducible. The fall and winter of 1921 were spent in desperate attempts to replicate the fleeting summertime success, ultimately rejecting Banting’s guiding experimental insight and turning to more conventional extraction methods. Given this, how should the pathbreaking impact of the original flawed experiment shape our judgment about best innovative scientific practices, in an era when reproducibility has become a scientific shibboleth?
Second, as much as insulin improved the lives of countless people with diabetes, many thematic aspects of living with diabetes remained resolutely constant: striving for control over the disease, managing the myriad self-care tasks, and addressing thoughts and feelings about responsibility for outcomes, desired or not. What do these enduring themes tell us about the goals of medicine, beyond reducing morbidity and mortality?
The final irony moves in the other direction: Given how remarkable insulin is (truly a veritable wonder of modern medicine), we should be struck by how taken for granted insulin has become. Our ability as a species to acclimate to miraculous advances threatens our ability to perceive how to best advance. How can we overcome this tendency, which threatens the misvaluation of science?
Patricia D’Antonio, the Carol E. Ware Professor of Mental Health Nursing and director of the Barbara Bates Center for the Study of the History of Nursing in the School of Nursing
It is hard to overstate the importance of the discovery of insulin 100 years ago. Almost overnight, a diagnosis that meant an inevitable death sentence for afflicted children became one transformed into an illness that could be successfully managed with both a new therapeutic and lifestyle changes. It marked both the bright promise of the new, laboratory-based scientific medicine, and the legitimation of nursing’s claim to more widely recognized specialized knowledge that ultimately resulted in state-based registration laws that protected their practices.
One needed to know how to prepare carefully calibrated hypodermic injections, monitor for over- or under-reactions to blood sugar regulation, and act in instances of untoward reactions to an intervention around which there was still uncertainty. But, in ways we are only beginning to understand, tensions quickly emerged—not between nurses and physicians but between nurses and nutritionists.
Who was best positioned to teach parents and children about the diets needed to stabilize glucose productions? Nutritionists, an emerging career for women in the opening decades of the 20th century, claimed the expert knowledge needed. But nurses, long trusted as what historians have called the “connecting link” between scientific knowledge and its practical applications, had the carefully won credibility and, as important, access to the families.
Nurses won this one historic battle: They successfully incorporated nutrition knowledge and teaching into their practices and assumed responsibility for teaching families about diabetic diets and other kinds necessary to achieve the full promise of laboratory therapeutics.
One hundred years later, of course, much has changed. Nurses and nutritionists work as interdisciplinary colleagues titrating families’ need for the generalized knowledge that nurses provide and the specialized knowledge that is the nutritionist domain. But these historical points where an important discovery demands something new of our healthcare system remain relevant. Who, for example, should knock on doors to encourage COVID vaccination? Our current literature speaks to the importance of “trusted messengers.” Our history suggests such messengers have always been nurses.
Mark Schutta, medical director at the Penn Rodebaugh Diabetes Center and the G. Clayton Kyle Associate Professor in Diabetes at the Perelman School of Medicine
Prior to Banting and Best’s groundbreaking work, caloric restriction served as the only means of prolonging certain death for diabetics. Like all uncontrolled diabetics in the early 1920s, a young boy known as J.L. was suffering from osmotic diuresis, a condition of relative starvation due to the absence of insulin and impaired ability to absorb and utilize glucose, the metabolized end product of food. In an effort to lower his glucose, J.L.’s kidneys excreted some of his glucose, taking water with it. This rendered J.L. chronically hungry, dehydrated and weak. In December of 1922, he weighed 15 pounds; three months later after receiving insulin he weighed a healthy 29 pounds. J.L.’s life was saved and his metabolism re-regulated because of Banting and Best’s achievement, representing one of the most impactful translational research endeavors ever accomplished.
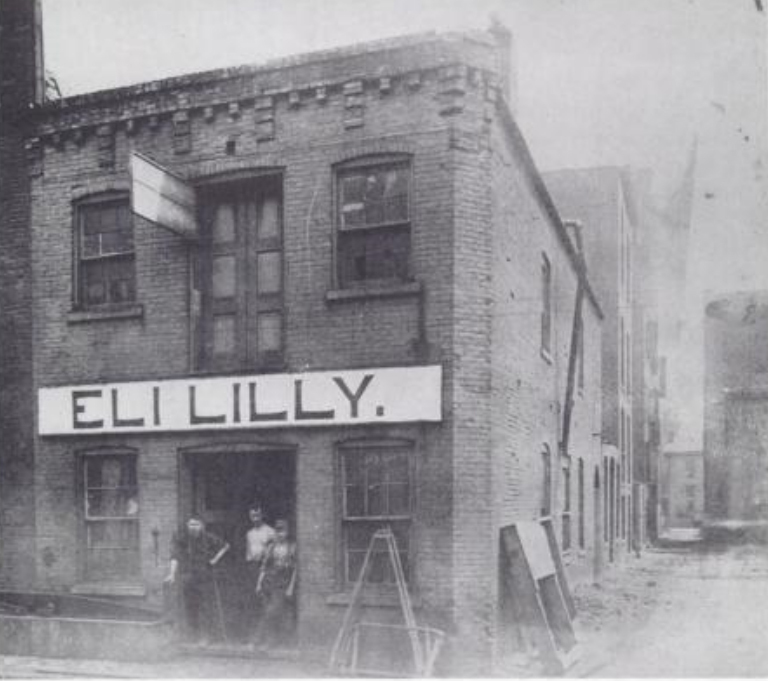
As news of the University of Toronto’s group spread worldwide, demand for their extract grew. To respond to this demand and improve their product, the team reached an agreement with Eli Lilly to establish a partnership. In an altruistic gesture on the part of the team, an American patent on both insulin and Toronto’s method of making it was awarded to Banting, Collip, and Best. For $1 each, the three discoverers assigned their patent rights to the Board of Governors of the University of Toronto. A patent ensured the potency and purity of the insulin and prevented other manufacturers from making ineffective versions.
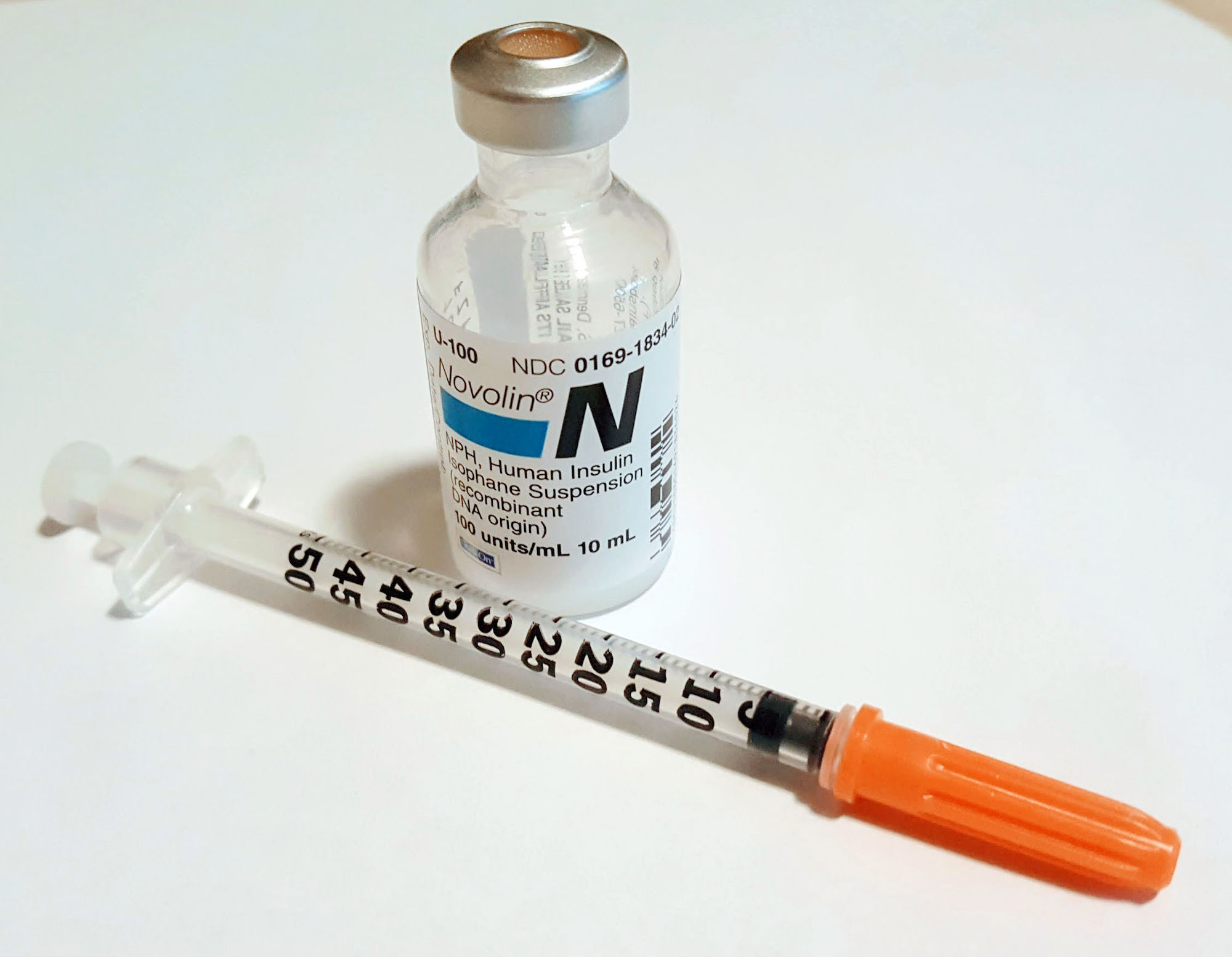
Gradually, improvements in purification and stability of the insulin brought the life-extending drug to patients everywhere. Today, patients and their clinicians are blessed with human insulin analogs which maintain an exquisite level of quality control and predictability. Life expectancy for Type 1 diabetics is now approaching non-diabetics.
Despite all of these improvements in diabetes care, the cost of modern insulin is often beyond the reach of many Americans who suffer from a completely treatable illness that is not their fault.
Tens of millions of lives have been saved and extended thanks to Banting, Best and Collip. They worked tirelessly to discover insulin but also sacrificed fortune in the interests of the common good. Their legacy is an example to us all.
Mark Pauly, Bendheim Professor in the Department of Health Care Management; professor of Health Care Management and Business and Public Policy at The Wharton School; and professor of Economics in the School of Arts & Sciences
Insulin is one of the most important biomedical innovations of the 20th century, and it has lengthened and enriched the lives of millions of people who suffer from diabetes. However, the economic issues surrounding financing of research and pricing serve to illustrate the tradeoffs and challenges in balancing innovation and affordability in medicines.
The possibility of treating diabetes by injecting insulin derived from animal pancreases was discovered by the Canadian scientists Banting and Best in 1921. They did not want the patent for themselves, but it was Eli Lilly and Company that organized large-scale production and introduction into the U.S., followed shortly by a Danish for profit-nonprofit collaboration now known as Novo Nordisk. At present these are still two of the largest suppliers of insulin to the U.S. market, but despite the passage of time there is still no generic insulin in this country.
Instead, firms making insulin have for decades followed a practice of improving both the product and its delivery, moving from pig or bovine insulin to human insulin to purified synthetic analogue insulin, developing injector devices and insulin pumps, and refining the product into both fast-acting and long-lasting types of insulin that are easier to use than standard insulin.
The good news is that management of diabetes not solely using insulin is now much more effective with fewer side effects than in 1921. The downside is that “evergreening” of insulin products with new patents for improved products has inhibited price-reducing generic competition. What has been most striking in recent years has been a pattern of rapid increases in prices for patent-protected products, doubtless fueled by the widespread and growing presence of insurance coverage for the drug, but with adverse financial consequences for consumers with less generous coverage and insurers trying to hold down costs.
The most recent development is one that may interfere with the gentlemen’s agreement among the few producers to limit price competition: the entry of Walmart, in conjunction with Novo Nordisk, to offer insulin at pharmacies in its super stores at much lower prices than the retail prices of branded products. Perhaps this will lead to a different and better mix between innovation and economy in the future.
Mitchell Lazar, the Willard and Rhoda Ware Professor in Diabetes and Metabolic Diseases and the Director of the Institute for Diabetes, Obesity, and Metabolism at the Perelman School of Medicine
For most of human history, a diagnosis of diabetes was a death sentence. Diabetics were known to have high levels of sugar in their blood and urine, and in 1910 the British scientist Edward Albert Sharpey-Shafer hypothesized that their bodies were unable to use the sugar due to the lack of a chemical made by the pancreas, which he termed “insulin.” Just over a decade later, insulin was discovered by Banting and Best, who worked with James Collip to purify insulin and make it available to patients. In January 1922, a 14-year-old boy named Leonard Thompson became the first person to receive an injection of insulin, which saved his life. It was truly a miracle of modern medicine.
Incremental improvements in insulin production, blood sugar monitoring, and insulin delivery have improved the length and quality of life for diabetics, and there is great hope for a cure using closed loop insulin delivery systems or cell-based therapies including transplantation of insulin-producing cells.
In 1921 most diabetes was due to the near complete absence of insulin, now referred to as Type 1. Over the past century, however, a different type of diabetes, called Type 2, has become nearly 20 times as common as Type 1 and is still on the rise, posing a major threat to human lifespan and health span. Type 2 diabetes is due to the inability of the body to respond normally to the insulin it produces, and is highly related to the epidemic of obesity, which is in turn due to changes in diet and lifestyle superimposed on our human genome that did not evolve to cope with a surfeit of nutrients. One hundred years ago, Type 2 diabetes was unheard of in children, and now it rivals Type 1 in its prevalence.
New discoveries are urgently needed to combat this scourge of the 21st century with the impact that the discovery of insulin has had in the history of Type 1 diabetes.
Terri Lipman, the Miriam Stirl Endowed Term Professor of Nutrition; professor of Nursing of Children; assistant dean for Community Engagement in the School of Nursing; and pediatric nurse practitioner in the Division of Diabetes and Endocrinology at the Children’s Hospital of Philadelphia
The discovery of insulin in 1921 was a watershed moment. Diabetes changed from a certain death sentence to a manageable disease. The wasting and death described in the first recorded description of diabetes almost 2,000 years ago by Areteaus of Cappadocia was a result of the body’s inability to produce insulin. Insulin has saved millions of lives and limbs no longer “melt to water,” as Areteaus noted. What have we seen in the 100 years since? Even with insulin treatment, diabetes can result in devastating long-term complications that include blindness, heart disease, kidney disease, circulatory problems leading to amputations and a markedly reduced life span.
Managing diabetes remains a very labor-intensive process requiring constant monitoring of blood glucose, food and activity along with administration of insulin. Markedly advanced diabetes technologies infuse insulin without the need for injections and continuously monitor blood glucose levels. Based on the availability of new tools to more precisely manage diabetes and almost create an “artificial pancreas,” diabetes management is easier, and diabetes complications are significantly reduced for many, but not all.
In 1921, insulin was available to few. One hundred years later, there are great inequities in access to insulin and diabetes technologies. My practice and research are centered on children with diabetes. Data from Children’s Hospital of Philadelphia, and many diabetes centers across the country, have shown that Black children and children from low-income families have poorer diabetes control, higher rates of diabetes complications, and are less likely to be treated with the latest advances in diabetes technology.
It is critical to recognize the impact of socioeconomic disparities and structural racism on the care of children with diabetes. Diabetes outcomes cannot be improved for all when there are significant unrecognized and unaddressed social barriers impeding the provision of complex and demanding care in the home. Working to develop community-based diabetes interventions to address systematic racism, and being prepared to fight the entrenched systems that are structured to disadvantage populations of color are essential in eradicating diabetes disparities.