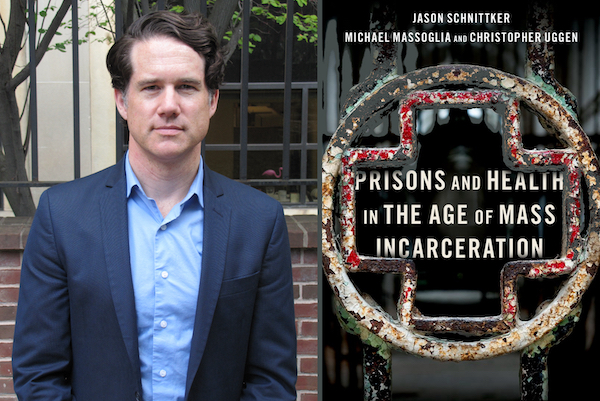
The following is an excerpt from “Prisons and Health in the Age of Mass Incarceration” by Jason Schnittker, Michael Massoglia, and Christopher Uggen (©2022 Oxford University Press).
At the heart of the relationship between prisons and health is a paradox. Prisons are charged with being punitive and therapeutic, with denying freedom and providing care. Common correctional concepts are replete with ironies. Protective custody, for instance, is a type of confinement where the intent is to shield those in prison from harm, especially from other people in prison.
But the idea is a contradiction if custody itself is harmful. And, indeed, incarceration is often harmful. The language of protective custody, for instance, is often used synonymously with solitary confinement, which is especially detrimental to well-being.
The paradoxes are apparent in other ways, too. In the spring and summer of 2020, more than 900 imprisoned Americans died of COVID-19, and thousands more will die of other causes. Prisons are implicated in the spread of other infectious diseases as well, including, at least historically, HIV and tuberculosis. Physical and sexual abuse are not uncommon in prison environments, leading to emotional and physical harm.
At the same time, though, many people in prison receive urgently needed health care, and they receive care they likely would not have received prior to incarceration. For many, incarceration increases their access to medical treatment, leading to meaningful improvements in their health and risk profile, from more accurate diagnoses of long-standing problems to better blood sugar control and reduced blood pressure. For young Black men, mortality in prison is lower than mortality outside of prison.
The paradox at the heart of prison health care has, if anything, grown sharper over time.
While medicine has expanded the range of therapeutic technologies, and concepts of appropriate punishment have evolved, the legal system has failed to provide guidance for what prisons are obligated to provide with respect to health care, making the tension at the heart of the system even more fraught. The tension is heightened further by the seemingly sharp but actually porous boundaries of the prison system’s remit. Whatever care prisons are able to provide to those in their custody ends abruptly at their release, even as the health of those previously in prison grows worse and better access to care would aid their rehabilitation.
Understanding the connection between prisons and health requires us to hold both of these ideas at the same time: prisons can undermine health and provide meaningful health care services, and they operate in an environment that insists on both. Understanding the connection also requires us to understand the prison system as a complex institution, operating under a varied set of legal, cultural, and political mandates.
As an institution, the prison system ostensibly serves the interests of criminal justice. As with many other institutions, however, prisons are increasingly bound up with a variety of coexisting and often incompatible goals. Prisons are required simultaneously to supervise, punish, correct, and maintain the health of those in their care. The same personnel often serve all these functions at once.
Given these mandates, there are important distinctions between what prisons are obligated to do, are allowed to do, and actually do. In addition, prisons intersect with other institutions charged with the care of similar populations, albeit with different responsibilities and operating principles. At present, for instance, the U.S. prison system provides a good deal of care for those who, in an earlier era, might have been treated in a psychiatric hospital. By some accounts, jails can now be regarded as America’s largest system of psychiatric hospitals.
But the legal mandate that undergirds health care in prisons sets prisons apart from other care-providing institutions. At root, prisons are inimical to health. The law stipulates that U.S. prisons must provide health care, in keeping with the Eighth Amendment’s prohibition against cruel and unusual punishment. But the constitutional mandate that supports prison health care is far different from the ethic of care that governs normal health care encounters.
Unlike hospitals or clinics, prisons are largely defined by punishment. This, of course, is obvious. Punishment is what most people associate with prisons. Prisons involve cells, restraints, supervision, and serving time. And prisons sometimes are involved in state-sanctioned killing, as in the case of capital punishment.
Health is the antithesis of punishment. To punish is to harm and wound, whereas to care is to heal and cure. To discipline is to strip away, whereas to treat is to build up. Guards impose passivity, whereas physicians intervene to allow activity. It is difficult to imagine respecting an oath to first do no harm when the institutional prerogative is to penalize.
When judges sentence people to prison, they do so under the assumption that the experience will be painful. Some judges go a step further: they believe a prison sentence should be not only painful in itself—as if the forceful separation from loved ones and severe restrictions on freedom are insufficient—but also additionally painful, such that the material and social conditions of prison life should not be at all conducive to well-being. Some prison and jail officials even boast about the pains they inflict, as when they have no air conditioning in the summer heat, no pay for labor, and food costs of pennies per day.
To be sure, the philosophy behind incarceration has shifted over time. Strict punishment was not always the guiding philosophy. It is possible, for instance, to regard a prison sentence as an opportunity to rehabilitate people, as we did much earlier in our nation’s history. It is also possible to regard prisons as a place to provide people with the skills necessary for re-entry, as we did until relatively late in the 20th century.
Yet the present era has been defined primarily in terms of a get-tough approach, as well as a reluctance to extend to people in prison anything that might be considered an amenity. Tellingly, even the shared concept of “rehabilitation” is fundamentally different in prisons and hospitals. In corrections, rehabilitation denotes the elimination of offending, whereas in medicine it denotes improving and restoring capacities. In hospitals, rehabilitation is expansive, whereas in prisons it is restrictive. Rehabilitation becomes reducing recidivism or, even more reductively, reducing the cost to society once someone is released.
Yet the fact remains: The correctional system is plainly in the business of providing care.
Jason Schnittker is a professor in the Department of Sociology in the School of Arts & Sciences at the University of Pennsylvania. His co-authors are Michael Massoglia of the University of Wisconsin-Madison and Christopher Uggen of the University of Minnesota.
The text above is an excerpt from “Prisons and Health in the Age of Mass Incarceration” (©2022 Oxford University Press). Used with permission from the publisher.