This year’s flu outbreak is on track to be one of the worst in recent memory.
In a mid-February briefing, Anne Schuchat, acting director of the Centers for Disease Control and Prevention, noted a spike in overall influenza-related hospitalizations, and so far, 84 children have died from the flu. The peak, she added, could still be coming.
On top of that, this year’s primary flu strain, what’s known as H3N2, typically causes more severe disease, hospital admissions, and complications than other strains—particularly for kids and adults older than 65—and the current vaccine is having less success against it than usual.
“Overall effectiveness of the flu vaccine this year is estimated to be about 36 percent, although closer to about 25 percent for H3N2 strains,” says Ebbing Lautenbach, an epidemiologist and infectious disease physician at Penn Medicine. “The effectiveness of the flu vaccine varies by year depending on how closely it fits the circulating strains. But it’s typically in the 40 to 45 percent range.”
From year to year, the flu virus alters slightly. The mutations it acquires render it different enough to infect some people, but similar enough to strains from years’ past that many people’s immune systems “remember” it and can fight it off. Pandemic strains are more than just a little different and can spread rapidly through people who lack immunity to the new virus.
This is what happened in 1918, when the flu and flu-related complications killed tens of millions of people, many of whom were otherwise healthy individuals in their 20s and 30s. A century later, what has changed? Could something similar to the worst pandemic in history happen today? Researchers from across Penn are seeking answers, by monitoring animal influenza strains, studying how the immune system responds to the virus, and working to create more effective vaccines, in the hope of preventing such an outbreak in the future.
Point of No Return
To apply lessons from the Spanish flu, it’s important to first understand precisely how it spread. For Philadelphia, the point of no return harkens back to a single day and a single gathering.
In early September 1918, several hundred soldiers arrived from Boston into the city’s port, unknowingly bringing influenza with them. Despite an almost immediate appearance of the illness, Wilmer Krusen, then-director of the Department of Public Health and Charities, opted to conduct business as usual, offering only to begin a public campaign against coughing, sneezing, and spitting, nothing more.
His decision was bolstered by a declaration from Penn physician Paul Lewis, who claimed to have pinpointed Pfeiffer’s B. influenzae, a bacterium, as the disease’s cause—a fact later proved to be untrue. At the time, however, it gave the medical community false confidence that they now had a foe at which to direct their efforts, and events like the Liberty Loan Drive, aimed at selling millions in bonds to support the ongoing war effort, continued as planned.
On Sept. 28, 1918, 200,000 people gathered for the Liberty Loan parade, one of the largest in the city’s history. It wound through 23 crowded streets. Within days, hundreds of people had died and many more had fallen ill.
“The flu was here before then, it came in early September of 1918, but it was really on September 28 that it hit the city hard,” says Jessica Clark, an archivist at Penn’s Barbara Bates Center for the Study of the History of Nursing. On Oct. 3, after the flu killed 117 people in a single day—by some accounts more than the city’s weekly death toll from all causes combined—Krusen’s hand was forced. He banned all public meetings and closed all churches, theaters, and schools, finally acknowledging the grave threat.
Unfortunately, the damage had been done. The Daily Pennsylvanian, which had taken to reporting daily flu numbers, noted 636 new cases and 139 deaths on Oct. 4 alone. And the story continued to worsen. “The flu epidemic overwhelmed the Philadelphia medical system,” says Mark Frazier Lloyd, director of Penn’s University Archives and Records Center. “The hospitals in the region couldn’t handle it. They turned people away.”
‘Heroic Work’
At the center of it all sat a pair of health-care institutions, the Hospital of the University of Pennsylvania (HUP) and Philadelphia General Hospital (PGH). “You had two major hospitals back to back in West Philadelphia. HUP was for the people who could pay, and right behind it was the Almshouse, PGH, for people who could not,” Lloyd says. “By 1918, the buildings were cheek to jowl, and they had much the same physician staff.”
The war had drawn much of this crucial resource away from Philadelphia, however, with more than a quarter of physicians and an even greater percentage of nurses serving military duties, according to the Naval History and Heritage Command. Three-quarters of the hospitals’ medical and surgical staff were overseas. That meant a significant portion of the care fell to clinicians-in-training like Isaac Starr, who in 1918 was beginning his third year at Penn Medicine.
“Deaths in the hospital as a whole exceeded 25 percent per night during the peak of the epidemic,” Starr recalled more than 50 years later, writing in the Annals of Internal Medicine. “To make room for others the bodies were being tossed from the cellar into trucks, which, when filled, carted them away.”
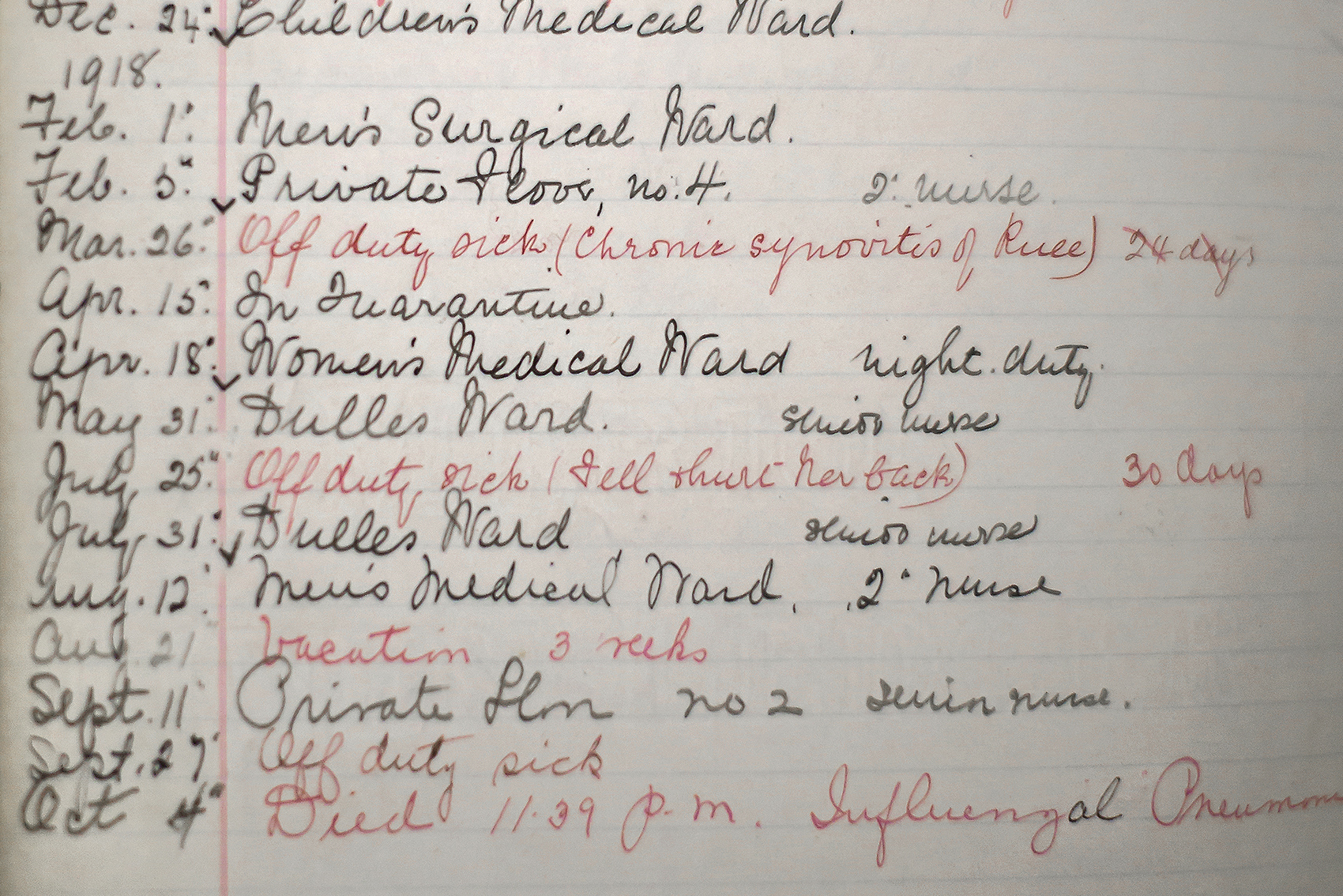
Student nurses also played a major role, says Patricia D’Antonio, director of the Bates Center and a professor at Penn Nursing. Page after page of nursing manager ledgers from the period, which note individual schedules, indicate nursing students falling sick from the flu. In the most striking examples, the final entry reads some version of this: “Oct. 4th, Died 11:39 p.m., Influenzal [sic] pneumonia.”
“Hospitals were filled to overflowing. People learning to be nurses who were taking care of these patients, they died,” D’Antonio says. “We don’t know who they were or how many, but nursing’s prestige rose dramatically in what was seen as heroic work during the flu, irrespective of the threat to their lives and well-being.”
The 1918 annual report from Hospital of the University of Pennsylvania describes the period’s chaos in honest detail:
The crisis caused by the influenza epidemic began in the early autumn and continued for about six weeks. The hospital immediately became overcrowded and the hospital staff overworked. The staff had been depleted by the absence of a large percentage of surgeons and physicians and nurses with the national forces. We therefore had to meet unexpected conditions of the utmost severity hardly more than half-staffed. But that we passed through these conditions without disaster was due to the unremitting zeal and self-sacrifice of doctors and nurses.
Part of the fear and uncertainty derived from the fact that this version of the flu was affecting populations not typically vulnerable to such a disease: otherwise healthy men and women in their 20s and 30s.
“The flu never had been a death sentence,” D’Antonio says. “Normally, then as today, flu struck infants, the immunocompromised, the elderly. This pandemic struck young men and women at the prime of their lives, and attacked the respiratory system creating all sorts of complications like pneumonia.” All told, some 50 million people died from the 1918 pandemic, half of which were young adults.
Preventing Future Outbreaks
Prevention is the best medicine, so the saying goes, and the biggest weapon in the arsenal against influenza—one decidedly unavailable in 1918—is vaccination. Many Penn researchers, like biologist Joshua Plotkin, are working on approaches to improve seasonal vaccines. One obvious strategy is to better predict which flu strain will likely rise to prominence in a given year.
Plotkin uses mathematical models to study the evolutionary forces at work in shaping seasonal flu outbreaks. In one line of research, he and colleagues examined 40 years of historical flu data and noted that viruses often acquire not just a single mutation that enables them to infect humans, but rather consecutive mutations that become problematic only in combination. “This informs vaccine choice because it seems some mutation sites are co-evolving,” he says. “If we know which pairs are likely to go together, we might be able to anticipate the epidemic strains that will emerge in a given year.” That’s a question for future research.
Changing the way vaccines get manufactured may also improve their efficacy. Currently, chicken eggs initially play host to the vast majority of annual flu vaccines. The World Health Organization analyzes global data to recommend the viral strains to be included in the vaccine for the following year, and these strains then get injected into eggs to multiply. The problem is that in the egg, the virus doesn’t replicate precisely; instead, it evolves and adapts to its environment. According to research published in Proceedings of the National Academy of Sciences in November 2017 by Penn microbiologist Scott Hensley, these “egg-adapted” strains can change to the point that they offer limited protection against the circulating virus.
“The problem in some cases may be that the intended strain of vaccine is well-matched to the circulating virus,” Hensley says, “but when the vaccine is actually produced, the viral antigens are changed in that process.” Though alternative techniques exist to manufacture vaccines, an overall shift would require substantial investment by the pharmaceutical industry.
Whether vaccinated or not, some individuals suffer more than others from certain influenza strains. Hensley, in collaboration with Plotkin and others, has recently shed some light on this mystery, showing that the very first strain of influenza a person encounters—often in infancy or childhood—shapes how that individual’s immune system will react to strains of flu encountered later in life. This may explain why, in 1918, individuals in their 20s and 30s paradoxically bore the brunt of flu-related mortality.
“It’s been proposed that we saw a lot of death in otherwise healthy individuals because the 1918 flu was highly inflammatory and their immune systems over-responded,” Hensley says. “But we think that the unusual age distribution might not have to do with the 1918 virus per se, but due to prior exposures that individuals had in the 1890s. [Perhaps] individuals were more vulnerable because their immune systems had been trained to respond to a very different type of virus.”
Similarly, a vaccine’s effectiveness comes down to how a person’s immune system responds to it. But what if instead of getting a new flu vaccine annually, a person could receive a single dose or a series that would protect against a broad swath of influenza viral strains, including those that haven’t even evolved yet? Such a strategy could also, theoretically, offer protection against a pandemic strain.
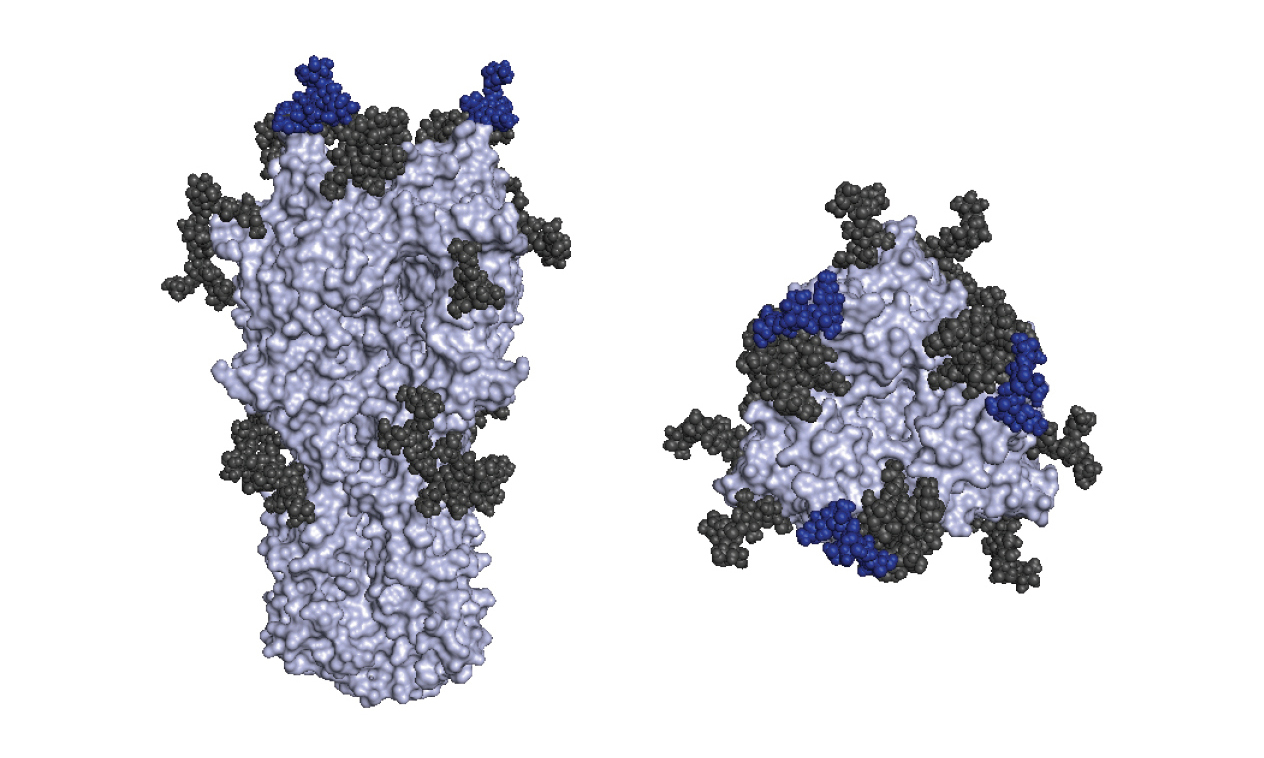
For many diseases—consider polio, diphtheria, and a host of other vaccines for infants and young children—this is already how it works. Yet a universal vaccine has proven elusive for flu, and the culprit is the shape-shifting influenza hemagglutinin protein, which mutates rapidly. “A universal vaccine would certainly be the golden fleece of the influenza vaccine world,” says vaccine expert Paul Offit of the Children’s Hospital of Philadelphia and Penn Medicine. “But I would settle for a much better seasonal flu vaccine.”
Offit, who co-invented the rotavirus vaccine commonly given to infants in the U.S., notes that efficacy rates of the seasonal flu vaccine range from 40 to 60 percent, and dip much lower some years. “A couple of studies have come out recently using novel strategies to create a vaccine; both were promising,” he says. “What we need is a vaccine that is biologically different from what we’ve done in the past.”
The Future of Flu
Barring a new vaccination strategy, one of the best available tactics to prevent a pandemic from taking hold is surveillance of circulating viruses, including those that exist in animal populations. At the School of Veterinary Medicine’s New Bolton Center campus, an arm of the Pennsylvania Animal Diagnostic Laboratory System (PADLS) exists to do just that.
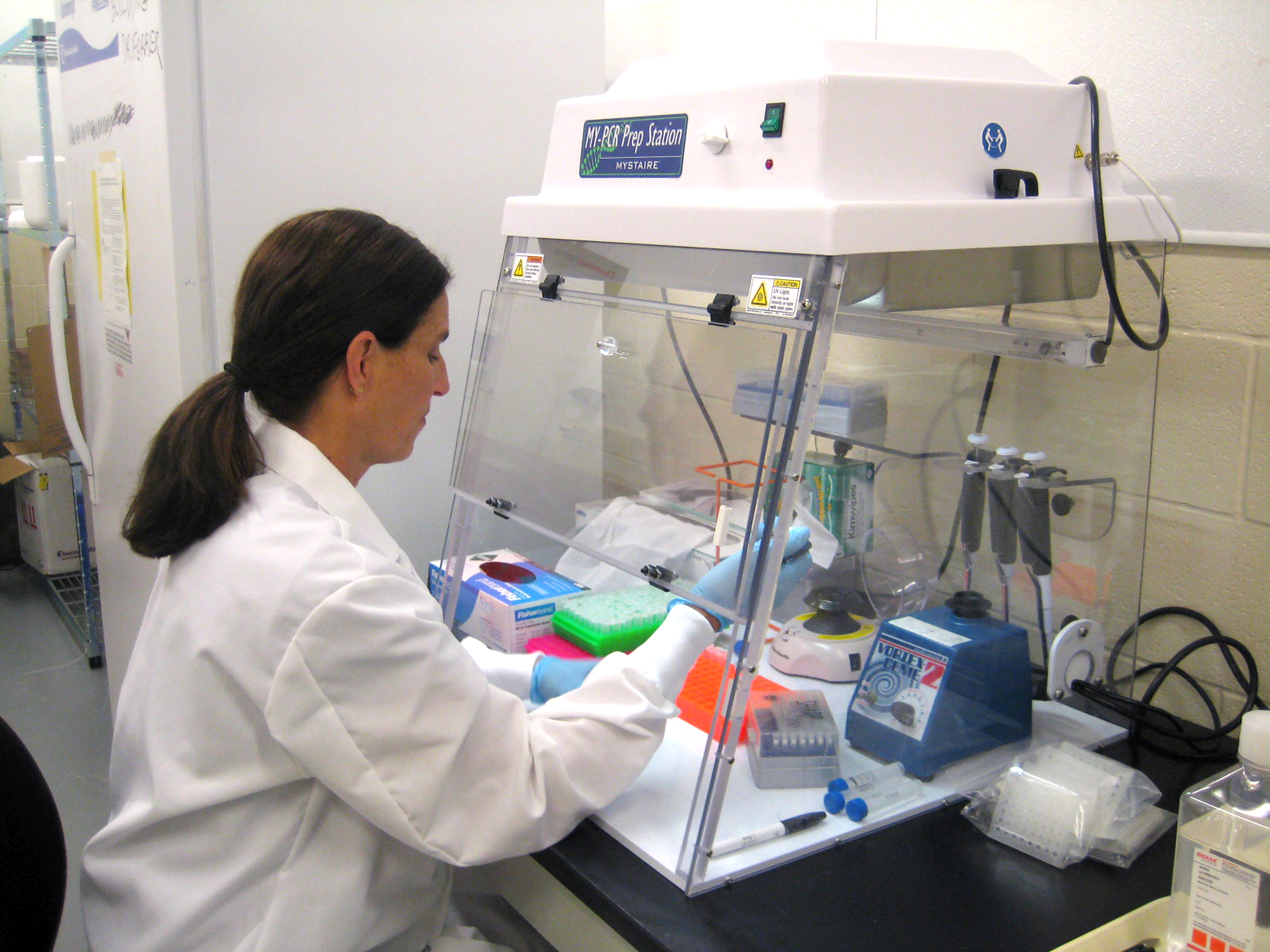
Together with labs at Pennsylvania State University and the Pennsylvania Department of Agriculture in Harrisburg, Penn Vet scientists monitor animal pathogens including avian influenza. Samples come largely from Pennsylvania farms, which voluntarily participate, though backyard chicken owners also submit samples, and the lab occasionally evaluates wild birds that are found dead. In 2016, the lab tested more than 50,000 samples for avian influenza, using assays that either look for antibodies or directly detect the virus itself.
Results that reveal the presence of an H5 or H7 influenza, the viral subtypes that are more likely to be highly pathogenic, get sent out for further testing, and PADLS collaborates with industry and the U.S. Department of Agriculture to ensure a rapid response, including quarantining the farm where the sample originated to contain the infection.
“The more rapidly and frequently you test, the less likely a potentially problematic virus is to spread,” says Michelle Lucey Gibison, who heads the molecular diagnostic laboratory service at PADLS-New Bolton Center. “The last thing you want is for these strains to spread.”
A highly pathogenic strain can have a significant, even devastating, effect on agricultural producers, says toxicologist Lisa Murphy, resident director of PADLS-New Bolton Center. “As a veterinarian, this is definitely an animal health issue. Birds may be euthanized if they test positive, even if they may not be showing significant illness. Along with that, there is an economic impact, and even a psychological or emotional impact to farmers. These are more than just chickens to them.”
And though the risk of a pandemic strain emerging from a bird population is relatively low, regular monitoring can give public health officials a head start on responding to a potentially dangerous pathogen.
‘When the Next Pandemic Comes’
One hundred years later, the world—and our health care system—is in a very different place than when the Spanish flu wreaked havoc on millions. Hospital infrastructure is greatly improved, and antibiotics exist to limit mortality from pneumonia, which ultimately killed many in 1918. But international travel is far more commonplace, enabling a lethal virus to ferry itself around the world in the noses of unwitting air travelers.
To that end, today’s vaccine is still currently the best bet against the flu, even with lower-than-normal efficacy rates. “The symptoms of flu this year are fairly typical: fever, headache, muscle aches, fatigue, specific respiratory symptoms like cough, sore throat, and nasal discharge,” Lautenbach says. “And even with a lower effectiveness of the vaccine, it’s still important to get vaccinated. Even a vaccine that doesn’t prevent disease can still reduce severity of illness.”
The majority of the people in modern times who die from the flu haven’t been vaccinated, Hensley says.
“We have antibiotics, and we do have better health care in general, but even this moderately severe flu season has really maxed out our health care system,” he adds, noting the temporary tents hospitals in some parts of the country have erected to manage flu-related patient overflow. “We should take a good look at what we have and how we could do better when the next pandemic comes.”
Because for those who study influenza, it’s not a question of whether another pandemic will happen but when. Before it does, however, lessons from a century ago will continue to shape the work of researchers at Penn and elsewhere who are trying to prevent anything from surpassing 1918’s outbreak as the worst flu pandemic the world’s ever seen.
Jessica Clark is an archivist at the Barbara Bates Center for the Study of the History of Nursing in the School of Nursing
Patricia D’Antonio is the Carol E. Ware Professor in Mental Health Nursing, the chair of the department of family and community health at the School of Nursing, and director of the Barbara Bates Center for the Study of the History of Nursing
Michelle Lucey Gibison is head of the molecular diagnostic laboratory service at the School of Veterinary Medicine’s PADLS-New Bolton Center
Scott Hensley is an associate professor of microbiology in the Perelman School of Medicine
Ebbing Lautenbach is the Robert Austrian Professor and chief of the division of infectious diseases at the Perelman School of Medicine
Mark Frazier Lloyd is director of the University Archives and Records Center
Lisa Murphy is an associate professor of toxicology in the department of pathobiology at the School of Veterinary Medicine and resident director of PADLS-New Bolton Center
Paul Offit is the Maurice R. Hilleman Professor of Vaccinology at the Perelman School of Medicine and director of the Vaccine Education Center and professor of pediatrics in the division of infectious diseases at the Children’s Hospital of Philadelphia
Joshua Plotkin is a professor of biology in the School of Arts and Sciences
Photo at top: A women’s ward in the Hospital of the University of Pennsylvania, circa 1903. Patients unable to pay for their hospital care would’ve come to such a place. When the flu pandemic arrived 15 years later, HUP was at the forefront of providing care to the city.