
Image: Kindamorphic via Getty Images
Someone who binge eats consumes an objectively large amount of food while feeling a loss of control over eating. When episodes occur weekly for several months, the action moves into the realm of binge-eating disorder. So how does this type of eating affect people with Type 2 diabetes and obesity who are actively working to lose weight?
According to new findings from the University of Pennsylvania published in the journal Obesity, it presents a significant obstacle: Those who continue to binge eat while trying to lose weight drop about half as much as those who don’t or those who do and then subsequently stop.
“Continued binge eating can act as a barrier to achieving success,” said Ariana Chao, an assistant professor in the Penn School of Nursing.
Chao studies how addictive-like eating behaviors influence treatment effectiveness for different populations. To better understand the role of binge eating in weight loss, she and colleagues from Penn’s Perelman School of Medicine, the Children’s Hospital of Philadelphia, the University of Connecticut and the National Institute of Diabetes and Digestive and Kidney Diseases assessed data from a study called Action for Health in Diabetes, or Look AHEAD. This multi-center randomized, controlled trial included more than 5,000 participants ages 45 to 76, all with a body mass index above 25 (or 27 for those using insulin) and Type 2 diabetes.
Look AHEAD’s original aim was to compare the effects on cardiovascular morbidity and mortality of two treatment options: an intensive lifestyle intervention designed to induce weight loss and diabetes support and education. The former included dietary recommendations, physical activity and behavior modifications; those in the latter group were encouraged to attend three sessions per year, one each about physical activity, social support and eating.
In addition, Look AHEAD annually assessed binge eating. Via a questionnaire, participants noted any instances in the past six months during which they consumed excess food and felt a lack of control over that consumption.
For this study, Chao and her team, which included Thomas Wadden, the Albert J. Stunkard Professor of Psychology in Psychiatry and director of Penn’s Center for Weight and Eating Disorders, analyzed the impact of binge eating on weight loss. The researchers found that at four years, participants who reported no binge eating or a reduced tendency to do so lost more weight than those who continued to binge eat. Participants lost 4.6 percent of initial body weight compared to 1.9 percent.
“Previously, it was unclear whether people who binge eat need to be treated for that behavior before attempting behavioral weight loss or whether they’ll do OK in behavioral weight loss without it,” said Chao, who has a secondary appointment in the Department of Psychiatry. “Our findings suggest that people who continue to binge eat after they start a behavioral weight-loss program need an additional treatment like cognitive behavioral therapy, which is one of the most effective for this condition.”
Such treatment includes work to recognize the interconnectedness of thoughts, feelings and behaviors, Chao said. For instance, if someone eats to cope with stress, CBT could aim to untangle why and how to change the behavior.
Though this study looked at a particular subset of people, two-thirds of the adult population in the United States is either overweight or obese. For that reason, Wadden said it’s important for clinicians to screen for these behaviors and, if found, refer those patients for additional care.
“Individuals with a history of binge eating shouldn’t be excluded or discouraged from engaging in behavioral weight loss,” he said. “But binge eating should be monitored regularly during weight loss. Participants who continue to report this may benefit from additional or more targeted treatment to ensure success.”
Primary funding for the study came from the National Institutes of Health, with additional support from the National Institute of Diabetes and Digestive and Kidney Diseases; National Heart, Lung, and Blood Institute; National Institute of Nursing Research; National Center on Minority Health and Health Disparities; Office of Research on Women’s Health; Centers for Disease Control and Prevention; and Department of Veterans Affairs.
Michele W. Berger

Image: Kindamorphic via Getty Images
nocred

nocred

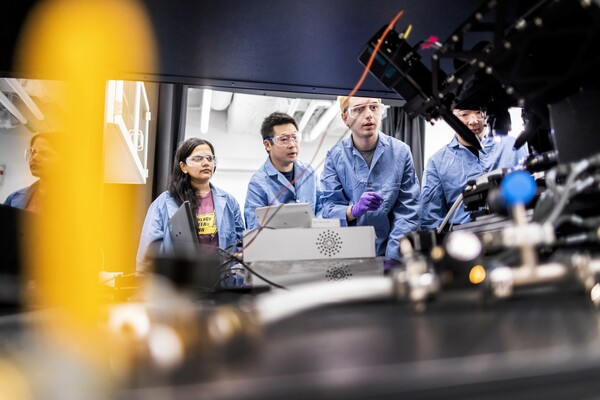
(From left) Kevin B. Mahoney, chief executive officer of the University of Pennsylvania Health System; Penn President J. Larry Jameson; Jonathan A. Epstein, dean of the Perelman School of Medicine (PSOM); and E. Michael Ostap, senior vice dean and chief scientific officer at PSOM, at the ribbon cutting at 3600 Civic Center Boulevard.
nocred