
Griffin Pitt, right, works with two other student researchers to test the conductivity, total dissolved solids, salinity, and temperature of water below a sand dam in Kenya.
(Image: Courtesy of Griffin Pitt)
One assumes that when a loved one moves to an assisted living facility or a nursing home, their needs for care are met by paid staff, relieving the burden on family and friends. A new study from Penn’s Leonard Davis Institute of Health Economics (Penn LDI), published in in Health Affairs, challenges that assumption, finding that family and friends continue to provide substantial amounts of care in these facilities, amounting to an invisible workforce, providing more than an extra “shift” of care every week in nursing homes and two “shifts” in assisted living facilities, on average.
Individuals living in residential care facilities are more likely to need care than their community-dwelling counterparts. To a large extent, unpaid family and friends are still helping to address their needs, despite the assumption that facilities have staff paid to do just that. Across a variety of types of care needs—household activities, mobility needs, and self-care—a higher percentage of individuals in residential care communities and nursing homes are getting assistance with these needs by informal care providers compared to their community-dwelling counterparts.
The findings help to explain the stories of staffing shortages and burnout in nursing homes under COVID despite no apparent drop in staff hours, when visitor bans were one of the first policy responses to the outbreak. The bans essentially eliminated this invisible workforce, increasing the care demands on the staff, on top of the extra work of the COVID protocols and infections themselves.
This story is by Norma Coe and Rachel Werner. Read more at Penn LDI.
From Penn LDI

Griffin Pitt, right, works with two other student researchers to test the conductivity, total dissolved solids, salinity, and temperature of water below a sand dam in Kenya.
(Image: Courtesy of Griffin Pitt)
Image: Andriy Onufriyenko via Getty Images

nocred
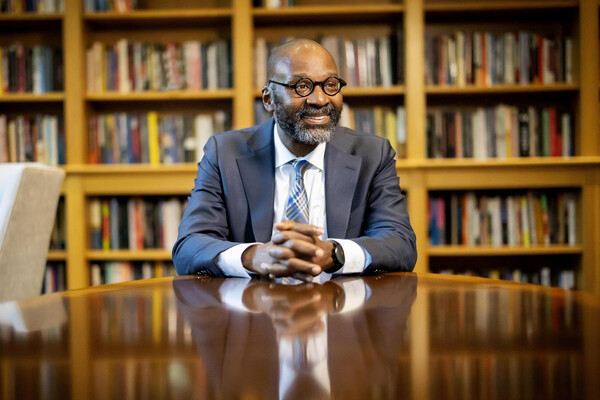
Provost John L. Jackson Jr.
nocred