
Griffin Pitt, right, works with two other student researchers to test the conductivity, total dissolved solids, salinity, and temperature of water below a sand dam in Kenya.
(Image: Courtesy of Griffin Pitt)
For the last 20 years or so, the U.S. has seen a significant increase in opioid and drug overdoses overall.
And while there was a slight leveling before the pandemic, “we’ve seen huge increases since COVID-19,” says Margaret Lowenstein, an LDI senior fellow, addiction medicine physician, and assistant professor of medicine at the Perelman School of Medicine. Overdose deaths topped 100,000 annually, setting painful records.
“Much of this is due to the rising prevalence of illicitly manufactured fentanyl, which is potent and deadly,” Lowenstein says. “We’re also seeing more stimulant-related overdoses involving drugs such as methamphetamines and cocaine.”
Some of that increase might involve people using multiple substances or drugs contaminated with fentanyl.
Another alarming development is the rising overdose rates in communities of color [Black and Hispanic], both in Philly and nationally. “Some of the increases are probably pandemic-related,” she said. “We’ve had social isolation, stress, economic instability, and physical illness, and we’ve also seen reduced access to services, treatment, and harm reduction.”
But a lot of marginalized people who lack access to technology lost touch with their care or returned to use during the pandemic. “It’s been a rough couple of decades, but these last couple of years have been particularly hard,” she says.
Lowenstein is seeing some positive solutions emerging in addiction treatment. “One big change I’m hopeful about is how the treatment system has been shaken up during the pandemic. A lot of regulatory flexibility emerged temporarily as part of the public health emergency. That allows for buprenorphine to be prescribed by telehealth and for less restrictive dispensing of methadone. The results so far are promising that these changes are largely safe and may be associated with better retention in care,” she says.
“This suggests that we need more flexible models of care that are patient-centered, that aren’t punitive, that allow patients to live and work, and don’t require perfect adherence because that’s more realistic for most people. But it’s unclear how much flexibility will persist.”
Lowenstein recently conducted a study of patients who were seen in Penn Emergency Departments (EDs) and received a naloxone prescription to prevent a future overdose. Her research team found one group was highly engaged in harm reduction and knew all about naloxone, but many others had little or no exposure to naloxone and little understanding about overdose risk and harm reduction.
“One of the things I’m interested in is these reachable moments for people who use drugs, like providing naloxone during an ED visit or using telehealth to prescribe medication treatment the same day patients ask for it,” she says.
“The health system is not always welcoming for people who use drugs. There’s a lot of stigma and trauma, so patients often don’t want to seek out care. So how can we engage the most at-risk patients? Can we find them in the community? Can we get them in the door via telehealth? A lot of the old models are punitive and come with the outdated sense that you need to jump through hoops or reach rock bottom to get treatment. But the evidence doesn’t support that. It’s better to engage people whenever you can and do more to help the people who aren’t getting to us.”
This story is by Karl Stark. Read more at Penn LDI.
From Penn LDI

Griffin Pitt, right, works with two other student researchers to test the conductivity, total dissolved solids, salinity, and temperature of water below a sand dam in Kenya.
(Image: Courtesy of Griffin Pitt)
Image: Andriy Onufriyenko via Getty Images

nocred
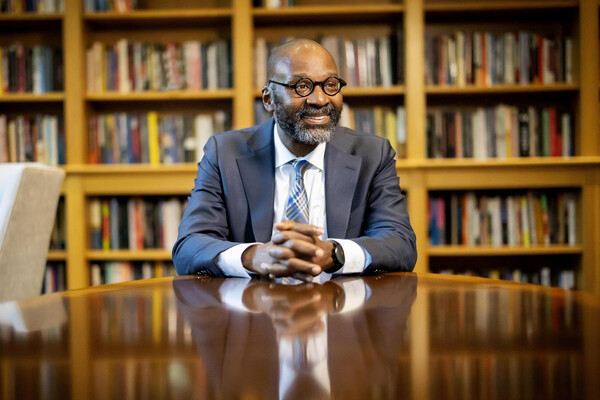
Provost John L. Jackson Jr.
nocred