
Griffin Pitt, right, works with two other student researchers to test the conductivity, total dissolved solids, salinity, and temperature of water below a sand dam in Kenya.
(Image: Courtesy of Griffin Pitt)
At clinics in towns just across the Ukrainian border in Poland, patients arrived one after another. Clinicians, some fresh out of school, were forced to make life-altering decisions for their patients at a rapid pace. Making matters worse, they had only a fraction of the clinical materials and tech that much of the world takes for granted, like CT scans that offer detailed images of inside the body. But a fresh view recently changed that—and it’s making a dramatic difference for Ukrainians in harm’s way.
Nahreen Ahmed, a physician with Penn Medicine, is an expert in training physicians and other care providers around the world in using ultrasound machines to assess injuries and other health concerns. Widely known as the technology that allows pregnant women and obstetric teams to see a developing baby inside the womb, ultrasounds can help clinicians gain insight into just about any area of the body.
Through training both in-person and virtually, Ahmed has taught hundreds of clinicians how to use ultrasound equipment in emergency areas, conflict zones, refugee settlements, and many other places with few resources. She has also provided training in acute and critical care for patients in dangerous and unstable settings around the world. Trainees include many who are currently working in Ukraine, in addition to others in areas of Asia, the Middle East, and South America. For these efforts, she recently received the Robert Suskind and Leslie Lewinter-Suskind Faculty Global Health Award, which honors a Perelman School of Medicine faculty member who exemplifies a lifelong commitment to improving global health and access to care through training partnerships.
Ahmed’s current career trajectory began in 2018 in the city of Dhaka, Bangladesh, a South Asian nation with a population of roughly 165 million. A second-generation Bangladeshi-American, Ahmed created the Bangladesh Ultrasound Initiative, which has now provided ultrasound training to more than 150 physicians working in resource-limited settings.
Ultrasound is a good fit for these settings, Ahmed said, because the technology is accurate, versatile, and highly portable.
While in Bangladesh, Ahmed traveled to the Kutupalong refugee camp, comprised mainly of Rohingya Muslims, an ethnic group brutally persecuted for their religious beliefs and displaced from their native home of Myanmar. Upon seeing the conditions, Ahmed transferred to the refugee camp—the world’s largest, numbering more than 700,000 Rohingya—to care directly for the people there.
“Dysentery and diarrheal diseases were huge problems,” Ahmed says. “Another major problem was PTSD, based on what they’d experienced. But they said they would rather stay in the camp—would rather die, in fact—than go back to Myanmar.”
Since then, the training Ahmed provides in ultrasound and in acute and critical care has taken her work to global conflict zones and mass-migration areas all over the world, including in Yemen, Gaza, Syria, Sierra Leone, Colombia, and Venezuela. The impact she provides, and her motivation to serve in unstable and dangerous areas, have left an impression on her colleagues.
Read more at Penn Medicine News.
From Penn Medicine News

Griffin Pitt, right, works with two other student researchers to test the conductivity, total dissolved solids, salinity, and temperature of water below a sand dam in Kenya.
(Image: Courtesy of Griffin Pitt)
Image: Andriy Onufriyenko via Getty Images

nocred
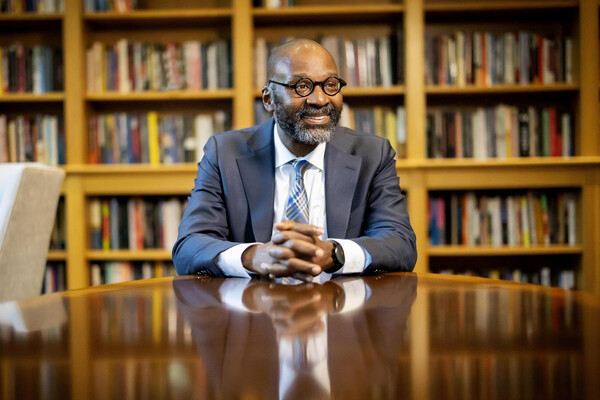
Provost John L. Jackson Jr.
nocred