
Griffin Pitt, right, works with two other student researchers to test the conductivity, total dissolved solids, salinity, and temperature of water below a sand dam in Kenya.
(Image: Courtesy of Griffin Pitt)
All potential transplant candidates undergo medical and psychosocial evaluations, which are crucial in determining whether they can get a transplant. The latter are meant to ensure that a patient has adequate social support and is committed to following the recommendations of their medical team. Psychosocial evaluations also consider a patient’s history of misusing alcohol or other substances, as well as factors related to their mental health. While this information is important to transplant success, psychosocial evaluations, like other measures in the transplant process, can lead to people of color facing worse outcomes.
Marina Serper, an assistant professor of medicine in the Perelman School of Medicine, discusses her recent study, “Racial and Ethnic Disparities in Psychosocial Evaluation and Liver Transplant Waitlisting” published in the American Journal of Transplantation.
“There is no gold standard for psychosocial evaluations, but it is generally agreed that they should be done in accordance with an internally consistent process that helps the transplant team decide whether a patient is a good transplant candidate,” Serper explains.
“In many transplant programs in the U.S., the Stanford Integrated Psychosocial Assessment for Transplantation (SIPAT), a questionnaire designed to assess psychosocial risk, is used as part of this process. If patients are found to be at high risk for complications from their answers, they may not be put on the waitlist to receive a transplant, even if they are good candidates physically. Such nonmedical reasons are important and may be valid, but also can introduce bias into the decision-making process.”
“SIPAT scores are supposed to aid centers in being more objective,” she says, “however, many of the items on the SIPAT are open to interpretation, and there are not agreed upon cutoffs that guide behavior at our center. My team is working on another project looking at the SIPAT tool to see which areas can be improved.”
“Importantly, issues of implicit bias are not resolved by the SIPAT. Transplant centers must be introspective and examine their decision-making processes.”
Serper’s research finds that Black patients have higher SIPAT scores on average, but they were also more likely not to be waitlisted than comparable white patients. “We also found that Black patients were more likely to be on Medicaid, to have lower levels of educational attainment, and to live in areas with poorer community health relative to white patients. These differences have unfortunately been previously shown in other settings,” she says. “In our research, we highlight that upstream determinants of health affect transplant access, which is life-saving for liver disease, and therefore further exacerbating health care disparities.”
Serper offers recommendations for policymakers to make the disparities smaller. “The first step clinicians must take is to recognize that health disparities exist. The second step is to ask what role their center is playing in reinforcing them and to brainstorm how they can reduce them by providing additional support. Group behavior and implicit bias are hard to discuss and disentangle but also have to be tackled,” she says.
“From a policy standpoint, a good starting point would be to follow the example of the United States Renal Data System. This collaborative network funded by the NIH collects information on the population prevalence of end stage renal disease and the proportion of patients on dialysis who have been added to the transplant waitlist. This type of detailed population data does not currently exist for either cirrhosis or primary liver cancer, which are both major indications for liver transplantation.”
This story is by Madison Weiss. Read more at Penn LDI.
From Penn LDI

Griffin Pitt, right, works with two other student researchers to test the conductivity, total dissolved solids, salinity, and temperature of water below a sand dam in Kenya.
(Image: Courtesy of Griffin Pitt)
Image: Andriy Onufriyenko via Getty Images

nocred
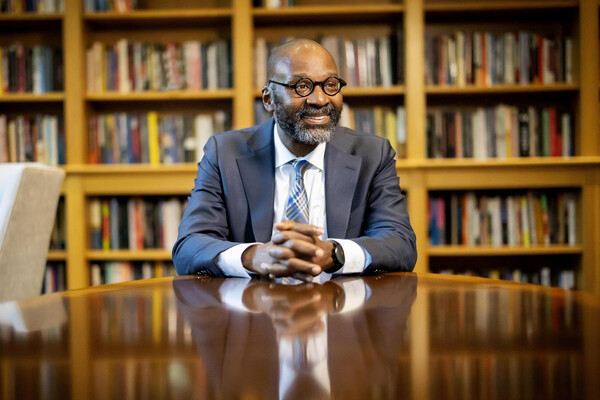
Provost John L. Jackson Jr.
nocred