
Image: Kindamorphic via Getty Images

As a year shaped by SARS-CoV-2 begins to wind down, the fact that Merriam-Webster’s “Word of the Year” for 2020 is “pandemic” showcases how much COVID-19 has impacted the lexicon.
Earlier this year, Penn Today published a list of key words and their definitions to help readers make sense of COVID-19. Now, as society gains a new level of understanding about the novel coronavirus and enters a new phase of the pandemic, Penn Today provides an update to that list outlining the language used in headlines, public health measures, and everyday discussions about COVID-19.
Spike protein: A protrusion on the exterior of a virus that allows it to bind to a cell. These proteins are what enable viruses to establish an infection in a host organism. In the most common illustration of the SARS-CoV-2 virus, the spike proteins are depicted as red protrusions dotted along the virus’ surface.
Incubation period: The time between when a person is exposed to an infectious agent and when symptoms first appear. The length of the incubation period depends on how long it takes the pathogen (a bacteria, virus, or fungus) to multiply and reach a minimum number and can also vary from person to person. For COVID-19, the median incubation period is approximately five days but can be as long as 14 days.
Viral shedding: When cells infected with a virus release newly replicated viruses into the body, which can then infect other cells or be expelled into the environment. For SARS-CoV-2, the primary route of expulsion is the upper respiratory tract, meaning that the virus can be released by talking, coughing, sneezing, and exhaling.
A person is considered infectious if he or she is still shedding virus. For COVID-19, the amount of virus present in nasal swab and saliva samples seems to peak in the first week after symptoms appear. Some people, however, have remained infectious for several months after diagnosis.
Positivity rate: The percent of diagnostic samples for a specific disease that come back positive. The value is calculated by dividing the number of positive tests within a specific time period, such as a single day, by the total number of tests within the same time period. The positivity rate does not measure the number of people in a population who have a disease but rather how many people who were tested have the disease.
The positivity rate is frequently used to assess how well a region is controlling the spread of disease. For COVID-19, the World Health Organization (WHO) recommends a positivity rate of less than 5% as an indicator of effective disease mitigation. As of the publication of this glossary, the positivity rate in the United States was over 10%.
R0 (pronounced “R-naught” or “R-zero”): Used to understand how contagious a disease is, this is the average number of people who will contract the disease from one infected person. A R0 of less than one means that every person who has the diseases passes it along to fewer than one other person on average; this suggests that the disease will dwindle and eventually die out.
Extremely contagious diseases, such as measles, have an R0 from 12–18, while seasonal flu strains have R0 values from 0.9–2.1. Studies of SARS-CoV-2 indicate that its R0 ranges from 1.8–3.6, similar to the coronavirus that caused the 2002–2004 SARS epidemic but higher than the seasonal flu. R0 is also known as the “basic reproductive number.”
R0 values are not static; they can be reduced using public health measures, such as isolation and quarantine, as well as personal behaviors such as mask wearing. Because the value of R0 can change over time, another related metric known as Rt, or the effective R number, can be calculated in real time as an outbreak progresses and used as a measure of how rapidly a disease is spreading.
Case fatality rate (CFR): Also known as the case fatality ratio, this metric is calculated by dividing the number of deaths caused by a disease by the total number of people diagnosed with the disease. A similar metric, known as the infection fatality rate (IFR), also includes an estimate of asymptomatic, undiagnosed cases as a way to account for undetected infections. The CFR and the IFR are both different from the mortality rate, which is the total number of deaths in an entire population.
In the 20 countries currently most affected by the pandemic, CFRs for COVID-19 range from 1.5% to 9.3%. These differences may be driven by testing capabilities, population demographics, and the capabilities of a country’s health care system. The CFR also varies based on age, with people 65 years or older more likely to die of COVID-19 than younger age groups.
Airborne transmission: The spread of a disease by particles that are small enough to remain in the air for extended periods of time and can travel a distance, generally greater than six feet, from an infected person. This is distinct from droplet transmission, caused by larger particles generated by coughing or sneezing that only travel a limited distance over a short time period before they fall.
While early evidence suggested that SARS-CoV-2 spread primarily by droplets, case studies in gym classes, choir practices, and restaurants suggest that airborne transmission can occur under certain circumstances. Current CDC guidelines now recommend avoiding “high-risk” indoor settings with crowding and/or poor ventilation where the virus can be more easily transmitted.
Close contact: A person who spent a total of 15 minutes or more within six feet of an infected person starting two days before that person experienced COVID-19 symptoms. While early guidelines defined close contact as a single 15-minute encounter, updated guidance changed this definition to include 15 minutes of total time spent with an infected person within a 24-hour time period.
Quarantine: The act of separating a person who may have been exposed to a disease from others until after the incubation period or after a negative test.
Isolation: The act of separating a person who has been diagnosed with an infectious disease from others to prevent the spread of the disease.
Sample: The biological material collected for a clinical test. For SARS-CoV-2, samples commonly used to detect active infections include a nasopharyngeal swab, a nasal swab, or saliva.
• A nasopharyngeal swab collects a sample from the back of the nose and throat. The “moderately uncomfortable” procedure involves a trained medical professional swabbing the back of the upper portion of the pharynx with a long swab.
• Nasal swabs only sample the lower portion of the nasal cavity and can be self-administered.
• Saliva samples require a person to spit or drool into a tube and can be self-administered.
Diagnostic test: A medical procedure designed to confirm whether someone has a disease or active infection. For COVID-19, there are two types of diagnostic tests: molecular tests and antigen tests.
• Molecular tests look for the presence of a virus’ genetic material. Tests for SARS-CoV-2 rely on reverse transcription polymerase chain reaction (RT-PCR), a laboratory procedure that amplifies small pieces of genetic material (in this case a portion of SARS-CoV-2’s RNA). These tests are highly sensitive and specific, meaning that they are able to detect small amounts of virus and do not often give false results when they use an appropriate cycle threshold (Ct).
• Antigen tests are designed to detect specific proteins that are present on the outer envelope of the SARS-CoV-2 virus. These tests can produce results much more quickly, cheaply, and at a larger scale than molecular tests. However, antigen tests have a higher probability of false negatives, meaning that a test result can come back negative when a person is actually infected.
Vaccine: A biological preparation that induces immunity to a disease without the person getting infected with that disease. There are different types of vaccines, but the goal of all approaches is to help the immune system recognize and destroy a specific pathogen.
The words “vaccine” and “vaccination” come from Variolae vaccinae (Latin for “of or from the cow”), the scientific name given to cowpox by English physician Edward Jenner. The cowpox virus causes skin lesions that can be passed from human to animal and is related to but much less deadly and contagious than smallpox. After discovering that milkmaids who had been infected with cowpox were immune to smallpox, Jenner developed a way to use cowpox pus to protect people against smallpox, a disease that was responsible for the deaths of approximately 300 million people in the 20th century.
RNA vaccine: A new type of vaccine that relies on messenger RNA (mRNA) to elicit an immune response. When the mRNA is taken up into a cell, the host’s molecular machinery makes a protein as instructed by the mRNA’s code. This protein stimulates an immune response that can destroy the virus if the person is exposed to it later. Two of the leading SARS-CoV-2 vaccines made by Pfizer-BioNTech and Moderna were developed using mRNA use the code for the virus’ spike protein.
Vaccine efficacy: The percentage of infections prevented in a group that’s been given a vaccine as compared to an unvaccinated group. To calculate a vaccine’s efficacy, a clinical trial is set up where one group receives a vaccine and the other a placebo. Researchers keep track of how many infections occur in each group. Efficacy is the relative difference between two fractions: The number of infections in the placebo group / total patients in the placebo group versus the number of infections in the vaccinated group / total patients in the vaccinated group.
Vaccine efficacy is reflective of how well a vaccine is likely to work on a population level. With the Pfizer/BioNTech vaccine, for example, 95% efficacy means that 95% of the people who receive the vaccine will be protected and 5% will not. According to CDC data, two doses of the measles (MMR) vaccine is 97% effective while three doses of polio (IPV) is 99 to 100% effective. On average, the seasonal flu vaccine is anywhere from 40 to 60% effective.
Emergency Use Authorization (EUA): During a federal state of emergency, the U.S. Food and Drug Administration (FDA) is authorized to approve products “to prevent, diagnose, or treat serious or life-threatening diseases or conditions that can be caused by a [chemical, biological, radiological, and nuclear] agent(s).” For a drug or device to receive an EUA, there must be data suggesting that it is “reasonable to believe” that the product “may be effective.”
In the U.S., SARS-CoV-2 was declared a federal public health emergency on Feb. 4. So far, EUAs have been issued for a number of COVID-19 test kits and therapies including remdesivir, monoclonal antibodies, convalescent plasma, the Pfizer-BioNTech COVID-19 Vaccine, and the Moderna COVID-19 Vaccine. The FDA issued and then revoked the EUA for chloroquine phosphate and hydroxychloroquine after new data showed that the drugs were “unlikely to be effective in treating COVID-19 for the authorized uses in the EUA.”
Cold chain: The equipment and logistics required to keep perishable products, including food, chemicals, and pharmaceuticals, at low temperatures during shipping. Because vaccines made from mRNA will degrade at room temperature, they must be stored at supercold temperatures (around -70° Celsius) for the Pfizer-BioNTech vaccine and -20° Celsius for Moderna) and require an “ultralow chain” for transport.
Any suggestions for additional words or phrases to add to the list? Please contact Erica Brockmeier.
Erica K. Brockmeier

Image: Kindamorphic via Getty Images
nocred

nocred

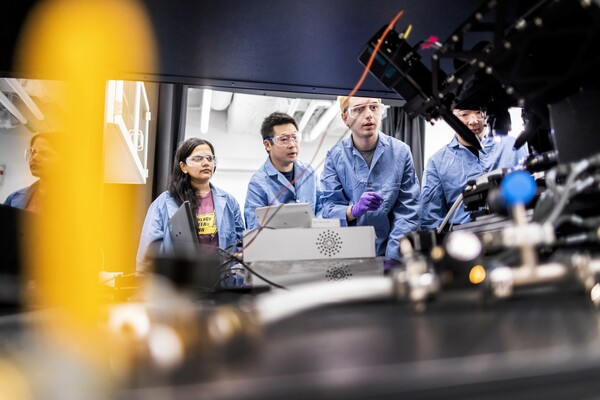
(From left) Kevin B. Mahoney, chief executive officer of the University of Pennsylvania Health System; Penn President J. Larry Jameson; Jonathan A. Epstein, dean of the Perelman School of Medicine (PSOM); and E. Michael Ostap, senior vice dean and chief scientific officer at PSOM, at the ribbon cutting at 3600 Civic Center Boulevard.
nocred